What is perianal fistula surgery?
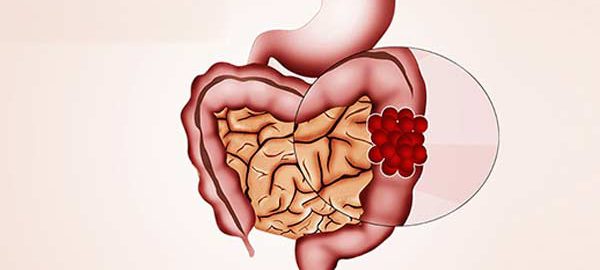
Most anal fistulas are the result of an infection that begins in the anal gland. The fistula forms a tunnel under the skin and connects to the infected gland. Surgery is usually necessary to treat a perianal fistula.
Previous considerations.
Before any surgery, an assessment should be carried out by the anesthetist where they will advise you which medication you should stop taking and which you should continue taking. Sometimes you must be evaluated by another specialist if you have underlying diseases.
In the case of anticoagulant treatment or treatment that facilitates bleeding, the anesthesiologist, haematologist, cardiologist or general practitioner must inform the attitude to be followed.
In the case of smoking, the habit should be stopped because it facilitates anesthetic management, smoker patients have more complications than smokers in anesthetic procedures.
It is recommended to perform moderate-intensity exercise before any intervention, unless there is a specific contraindication, such as walking at least 60 minutes a day.
How is the preparation prior to the intervention?
FOOD AND MEDICINE
In preparation for perianal fistula surgery, your surgeon may ask you to:
- Do not eat anything before surgery. You may have a sip of water with your medications, but avoid eating and drinking for at least six hours before surgery.
- Discontinue certain medications and supplements. Talk to your doctor about all medications and supplements you take. You continue to take most medications as directed by your doctor. Your doctor may ask you to stop certain medications and supplements because they can increase your risk of bleeding.
How is the surgery performed? (type of incision, resection, type of drainage, anesthesia)
BEFORE THE INTERVENTION
Perianal fistula surgery can be performed under general or spinal anesthesia. Numbing medications will be given intravenously in your arm or through a catheter in your spine. Once the medications take effect, the health care team will insert a tube down your throat to help you breathe if your case ultimately benefits from a general anesthetic. Your surgeon will then perform the surgery.
DURING THE PROCEDURE
Your doctor might recommend one of the following treatments:
- Removal of the perianal fistula (fistulectomy). Among one of the techniques that he can choose, the surgeon removes all the tissue that forms the fistula. Sometimes, removing the entire length of the fistula involves cutting the anal sphincter muscle, which is responsible for controlling gas and faeces leaks.
- Opening and cleaning of the perianal fistula (fistulotomy). The surgeon locates the tissue that forms the fistula, opens it, and cleans it. This option is less aggressive but with a greater possibility of reappearing the fistula.
What happens after the surgery?
After surgery, the patient slowly awakens from the effects of the anesthetic drugs, so they may have a feeling of not remembering the process. He will spend a short period of time in an area called post-anesthetic recovery, before being taken to his room.
HOW IS THE RECOVERY IN THE HOSPITAL?
It is possible to feel nausea or abdominal pain after the intervention but they will be controlled with the prescribed medication. After about 6 hours, you will begin with the intake of liquids and then solid foods. We recommend sitting down and starting to walk about 8 hours after the intervention. You will be supervised at all times by nursing staff.
If your surgery was performed in the morning and you have no previous illnesses, you may be discharged at the end of the day. If your surgery took place in the afternoon, you will usually leave the following noon.
HOW IS THE RECOVERY AT HOME?
When you are discharged home, you will be prescribed medication to make you feel as comfortable as possible. You will resume your previous medication following the surgeon’s recommendations, since some drug may not be recommended in the first days after surgery. It is essential to inform the patient that anal pain will be present during the first two weeks after surgery, so we will prescribe painkillers to control it. Sometimes you may need heparin injection to prevent the appearance of thrombi in your legs.
In relation to food, we recommend a diet rich in fiber (vegetables, salads, fruit…) together with an abundant intake of water to ensure that your stools are of a soft consistency and produce the least anal pain when defecating. You may need fiber or laxatives if you have significant constipation after the intervention.
We will recommend sitz baths with warm water and neutral soap several times a day and after defecation. This will ease your discomfort. Avoid using toilet paper. You will be periodically evaluated by nursing staff on an outpatient basis.
Walk every day and as you feel less pain, increase the time you dedicate to it. Avoid physical exertion until the surgeon assesses you.
Virtually full recovery can take approximately three to six weeks after surgery, depending on the characteristics of your fistula.
What are the risks of perianal fistula surgery?
The normal thing is that your intervention proceeds without incidents but you must know the potential complications.
Infrequent and frequent risks: Infection or bleeding from the wound, acute retention of urine, inflammation of the anus. Prolonged pain in the area of the operation. Phlebitis
Infrequent and serious risks: Significant infection of the anus and perineum. Incontinence to gases and even feces. Anus stenosis. Reproduction of the fistula.
These complications are usually resolved with medical treatment (medications, serums, etc.), but they may require a reoperation, and in exceptional cases death may occur.
Your risk of complications depends on your overall health and the reason you’re having fistula surgery.







 What is a skin lesion?
What is a skin lesion?